Secondary Billing
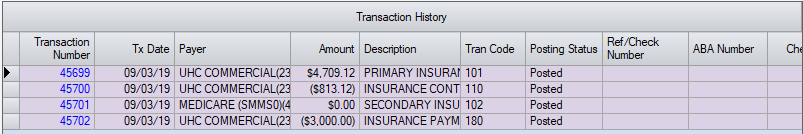
Once the primary charge has been billed, secondary or subsequent payers can be billed at anytime in HST Practice Management, but the most common practice is to bill when the primary payment and/or adjustment is entered.
In the Payments and Adjustments form, enter the Transaction Information for the primary payer, then enter the patient account number and select the appropriate visit. Enter the primary payment in the Applied Amount field. (This can be $0.00 if the primary allowable was applied to the patient's deductible.) Enter Contract Write Off if not applied at time of Charge Entry.
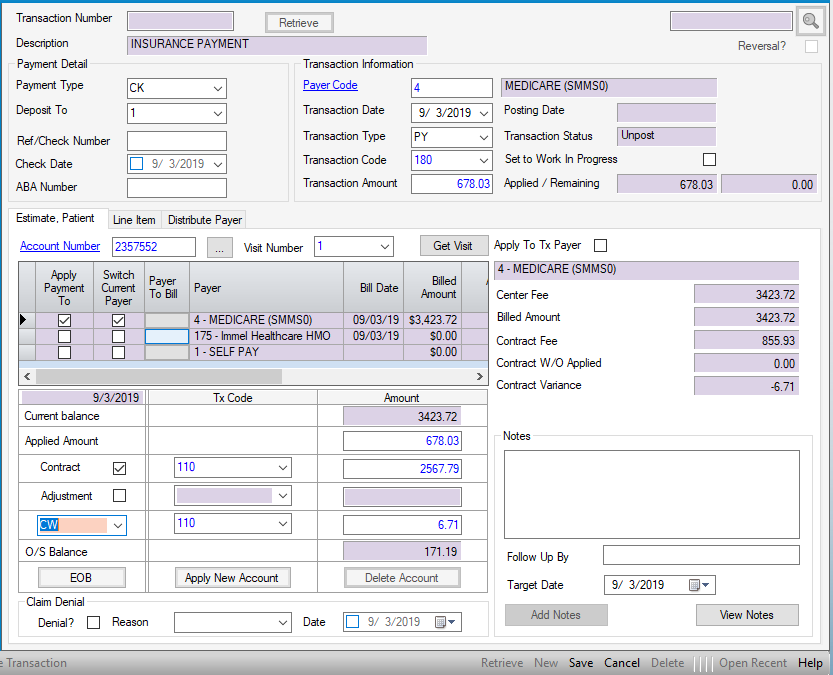
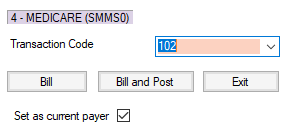
Select the grey function key (it will turn blue if the mouse is hovered over it to indicate it is an active function) to the left of the payer to bill in the Payer to Bill column. This will invoke the Secondary Billing form. If the primary and secondary payers are not in the same billing format (professional vs. institutional) and it is necessary to make changes such as adding diagnosis pointers, select  . This selection will invoke the original charge entry transaction to make the necessary changes prior to billing the secondary payer. If the formats are consistent from primary to secondary or subsequent payers, select
. This selection will invoke the original charge entry transaction to make the necessary changes prior to billing the secondary payer. If the formats are consistent from primary to secondary or subsequent payers, select  . This selection will Bill and Post the secondary transaction without any changes.
. This selection will Bill and Post the secondary transaction without any changes.
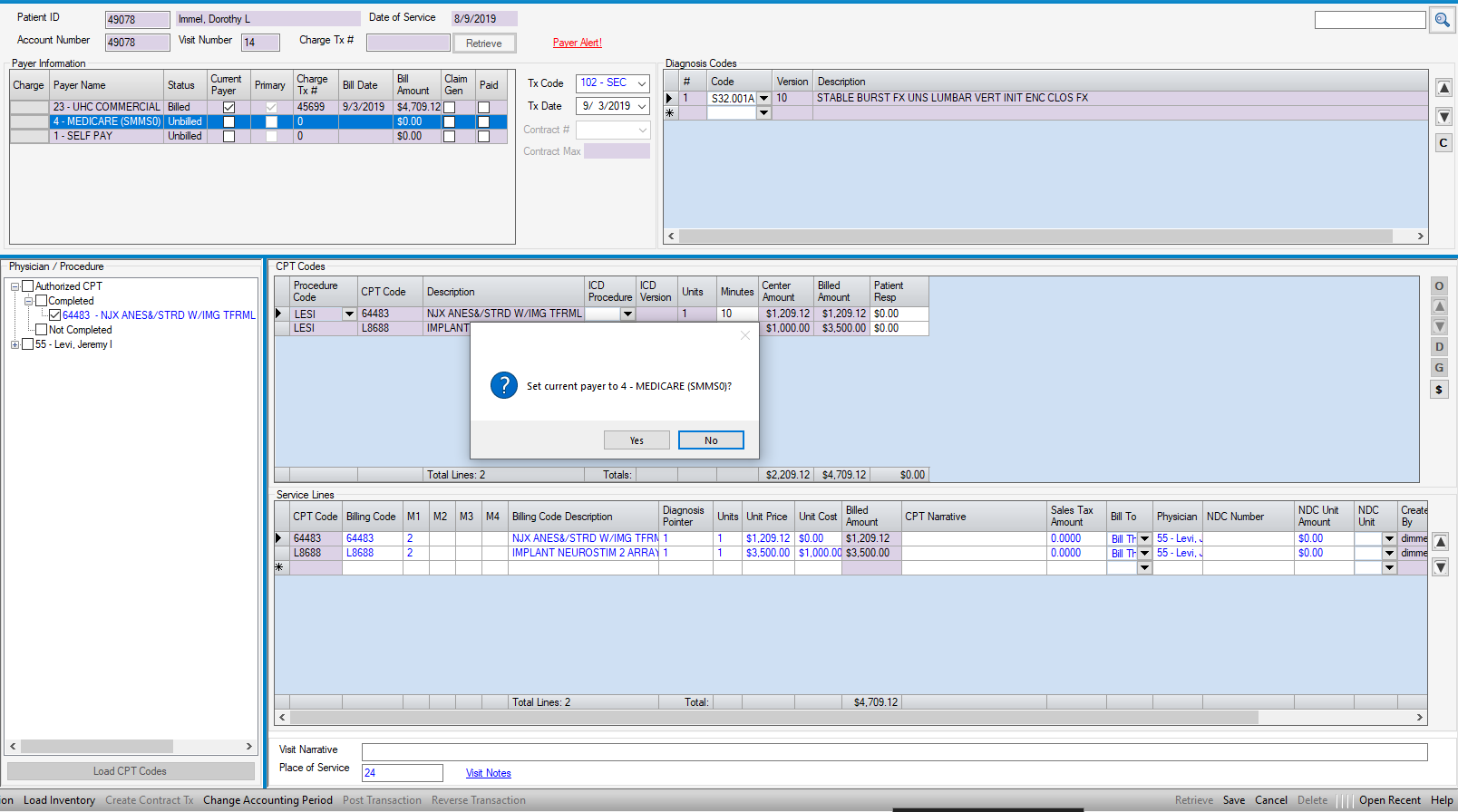
If  was selected, or if billing the secondary without posting a primary payment, retrieve the primary charge and double-click on the “Charge” cell in the Payer Information grid to the left of the insurance to be billed. This will put the form into ‘New’ mode and allow entry of diagnosis pointers or any other data that may be required to bill the secondary or subsequent payers. Once edits are completed and save selected, a pop up will ask whether to set the secondary as the current payer. To proceed, simply select yes.
was selected, or if billing the secondary without posting a primary payment, retrieve the primary charge and double-click on the “Charge” cell in the Payer Information grid to the left of the insurance to be billed. This will put the form into ‘New’ mode and allow entry of diagnosis pointers or any other data that may be required to bill the secondary or subsequent payers. Once edits are completed and save selected, a pop up will ask whether to set the secondary as the current payer. To proceed, simply select yes.
NOTE: To access the original charge transaction without posting a primary payment, select the blue hyperlink for that transaction in the Patient Account: Visit Ledger tab.
If billing the secondary electronically, The EOB - Explanation of Benefits must be completed and balanced prior to generating the secondary claim. This form can be accessed in Payments and Adjustments or in Patient Account: Billed Payers tab.