Other Configurations
Administration > Payer > Configuration
Billing Configurations such as suppressing statements, assigning default contracts, and restricting contract selection can all be set up on the Other Configurations tab in Administration > Payer > Configuration. In addition, State Reporting data such as Payment Source and NAIC can be added here as well as the NY Public Goods Mapping Categories.
Insurance Eligibility Configurations are also set up on the Other Configurations tab.
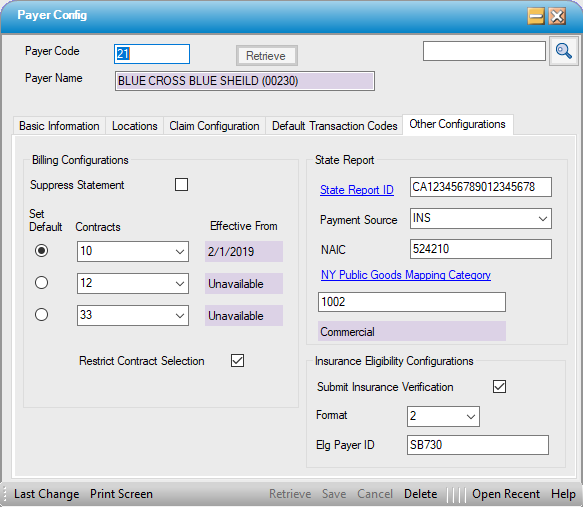
Billing Configurations
Suppress Statement
- Centers that have the Statement Triggers in Statement Options set to Due From Insurance will be sending statements to patients even when the total balance is still due from the insurance. Many states, however, prohibit sending statements to patients who have Medicaid plans or Workers' Compensation claims.
- To prevent statements from generating for payers whose guidelines prohibit billing the patient, check the Suppress Statement box under Billing Configurations on the Other Configuration tab of Payer Configuration for those payers.
Set Default
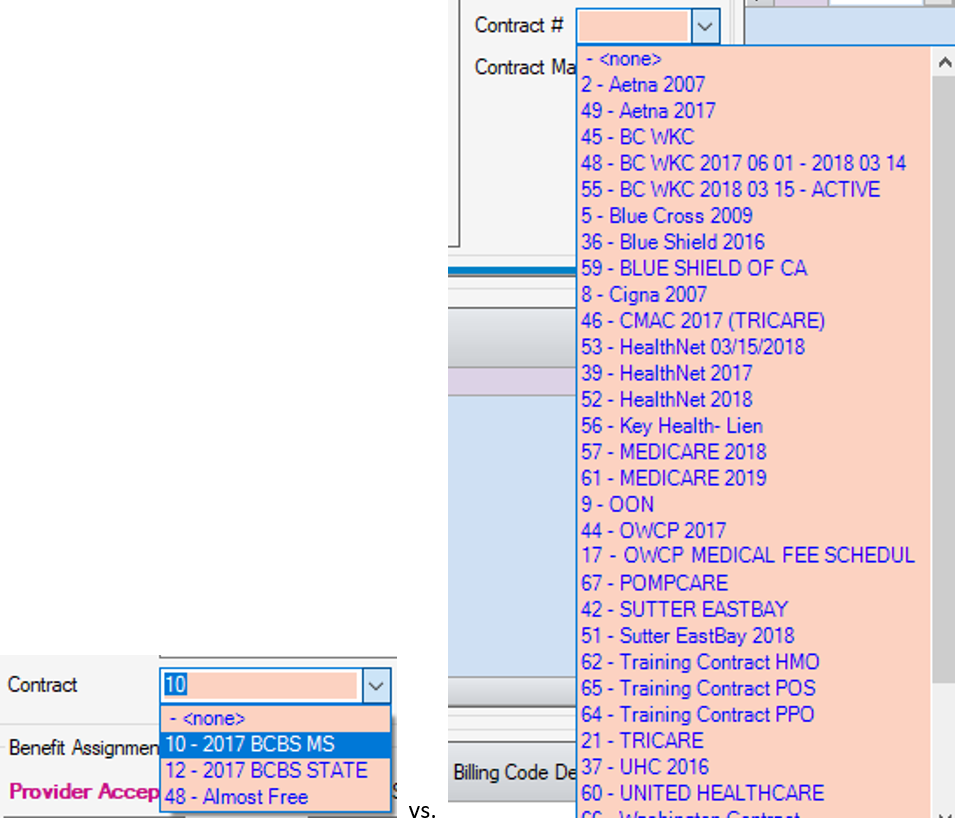
- Set Default - Selecting the Set Default radio dial of one of the up to 3 contracts entered (see below) will make the contract selected the default for this payer. The default contract can, however, be edited in either the Payer Information tab or Patient Estimate within Case > Registration > Insuranceor in Billing > Charge Entry.
- Contracts - Up to 3 contracts can be entered for each payer. Examples of how this may be used are as follows:
- A Payer may have different rates for HMO vs. PPO vs. POS plans. This option allows centers to build one payer and attach all 3 of those contracts rather than having to build 3 separate payers.
- As contracts expire and rates are renegotiated, both the old rates (contract that is expiring) and new rates (contract that is about to come into play) can be attached to a payer so that each contract is available for selection by the verifier who is running an estimate for a future dated visit or the biller who is entering or updating charges for an older date of service.
- Effective From - This is a read only field designed to assist in the selection of the default contract by providing the Begin DOS (if entered) from the Basic Information tab of Administration > Payer > Contracts Overviewso that the current contract can be selected as the default.
Restrict Contract Selection.
- Checking the Restrict Contract Selection box will limit the selections available in the drop down in the Payer Information tab or Patient Estimate within Case > Registration > Insurance or in Billing > Charge Entry to only the 1-3 contracts entered in this tab. If this check box is not checked, users will still have the ability to select from all active contracts.
State Report
- State Report ID - Enter the government assigned Payer ID (to appear on State Reports) or select the hyperlink to search by State Payer Code or Description.
- Payment Source - Select the Payment Source from the drop down. This is a Center Table that is created and maintained at the Center level in Administration > Code Table Maintenance.
- NAIC - The NAIC number is used for electronic claim billing. This number can usually be found on the patient's ID card or the clearinghouse web site.
NY Public Goods Mapping Category
- Use this hyperlink to search by NYPG Category or NYPG Code. This is an Enterprise Table created and maintained at the organizational level in Administration > Code Table Maintenance.
- The selection made above will then populate the next two fields with the NYPG Code and NYPG Category from the NY Public Goods Code Enterprise Table.
Insurance Eligibility Configurations
- Submit Insurance Verification - This check box must be checked to perform electronic verification for this payer (either Real Time or by batch).
- Format - The current format is 5010, so this drop down will default to 2 - 5010.
- Elg Payer ID - If the Payer ID for verification is different than the Payer ID for claim submission, the verification Payer ID must be entered here. If the number is the same, this field can be left blank as the interface will pull the information from the Claim Configuration tab.