Authorization Info
Case > Registration>Insurance > Authorization Info
The Authorization Info tab is accessed via the Registration quick launch icon  , Case>Registration>Insurance, or via the alternate search menu accessed by right clicking on the appointment in the appointment sheet or the patient's visit in any tree view and selecting the Registration>Insurance path.
, Case>Registration>Insurance, or via the alternate search menu accessed by right clicking on the appointment in the appointment sheet or the patient's visit in any tree view and selecting the Registration>Insurance path.
The purpose of the Authorization Info tab is to minimize claim denials by ensuring that all scheduled procedures that require an authorization have received confirmation that authorization has been approved by the payer prior to performing the procedure. In addition to this function, codes entered here can be pulled into the Patient Estimator for accurate profiling, and this tab also interfaces with the CPT codes entered in charge entry to insure that the codes authorized match the codes billed so that claims can be held and retro-authorizations obtained prior to billing when they do not.
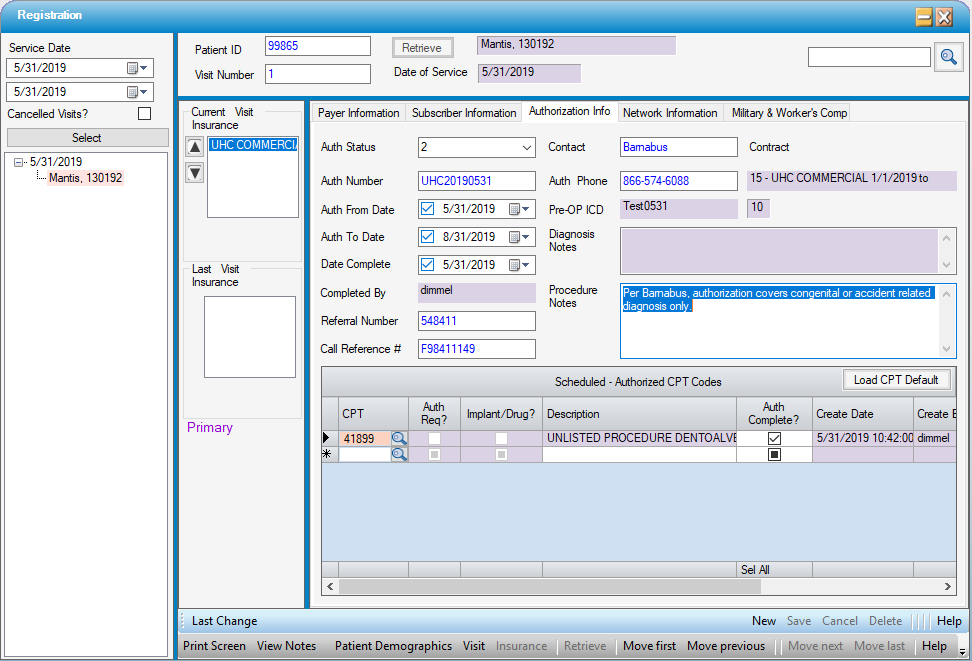
Payer Information
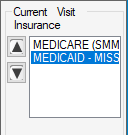
Though authorization is generally only required by the primary payer, Authorization Information can be entered for Primary, Secondary, or subsequent Payers. To select the correct Payer, double click on the Payer Name under Current Visit Insurance.
Auth Status will default to 0 - None. This status indicates that no action has been taken to confirm whether or not authorization is required or has been obtained. This status will prompt a Workflow Task if Primary Insurance Not Authorized is flagged for Inclusion in Workflow Configuration.
Available Auth Status selections are:
- 0 - None (default)
- 1 - Auth not required (no authorization is required for the scheduled procedure)
- 2 - Auth completed (authorization has been approved for the scheduled procedure)
- 3 - Auth Pending (authorization has been requested but has not yet been approved)
- 4 - Auth Denied (authorization was denied for the scheduled procedure)
-
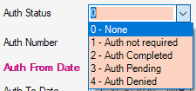
- Status 0 and Status 3 will both generate WorkflowTasks if Primary Insurance Not Authorized is flagged for inclusion in Workflow Configuration.
Once current status has been selected, the Authorization Number and relevant dates can be entered:
- Auth From Date
- Auth To Date
- Date Completed
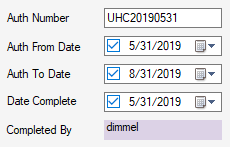
- Completed By is a read only field that will populate automatically with the user id when dates have been entered and saved.
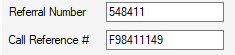
Additional fields are available to record both the Referral Number and Call Reference Number, if provided:
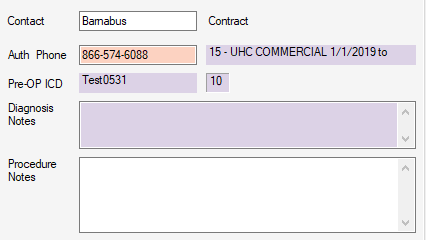
Users can also enter the Contact with whom they spoke at the Payer, or the web portal from which Authorization status was obtained. The Auth Phone number will default from Payer Configuration Overview: Location if an Authorization number was added. If not, it can be added in this field or default number can be edited.
The Contract is read only and defaults to the contract selected on the Payer Information tab. Diagnosis Notes are also read only and populate with any entries made on the Appointment. Procedure Notes will populate with entries from the Authorization Information tab on the Appointment, but these notes can be edited in this tab.
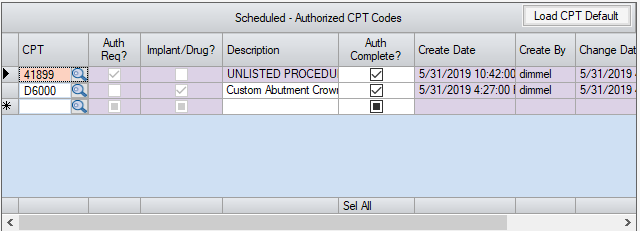
Scheduled-Authorized CPT Codes Grid
CPTs can be entered in the grid one of 4 ways:
- If CPT Codes were entered on the Authorization Information tab on the Appointment those codes will populate automatically but can be edited.
-
 will load all CPT Codes attached to a scheduled procedure in Procedure Configuration. Users can then delete any that are not relevant to the Authorization Info they are entering.
will load all CPT Codes attached to a scheduled procedure in Procedure Configuration. Users can then delete any that are not relevant to the Authorization Info they are entering. - CPT codes received from the surgeon's office can be typed in manually.
- The magnifying glass search option is also available to find relevant CPT Codes for procedures scheduled.
The Auth Req? column is a read only check box that will reflect whether the Auth Req? box was checked in the Contract Carve Outs Tab for the CPT Code entered.
The Implant/Drug? column is also a read only check box that will reflect whether or not the Implant or Drug CPT Category was selected in CPT Code configuration. Also, if the implant or drug check box was selected, the Description column will be open for editing. Otherwise, this will also be a read-only field.
The Auth Complete? check box is manually checked by the User to indicate all CPT codes for which Authorization approval has been confirmed. These codes will show up as Authorization Completed in Charge Entry.
Additional read-only columns are for tracking purposes: Create Date, Create By, Change Date, and Change By.
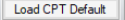
Patient Estimator
Any CPT codes entered in the Scheduled - Authorized CPT Codes grid can be pulled into the Patient Estimate by selecting the Authorized check box and the Load CPT Code function in that form.
Additional fees, such as for cosmetic procedures done in conjunction with a covered procedure, upgraded IOLs, or outstanding balances from previous dates of service can still be included when entering the Amount Due DOS.
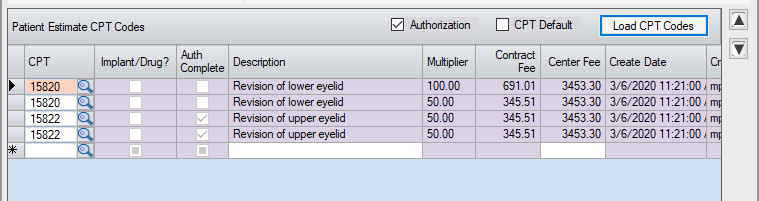
Charge Entry
Any codes entered in the Scheduled- Authorized CPT Codes grid will show up under Authorized Codes in Charge Entry. If the Auth Complete? box has been checked, they will fall under the Completed sub-heading. If the Auth Complete? check box was not checked, they will fall under the sub-heading of Not Completed.
If CPT codes are entered in Charge Entry that were not entered on the Authorization Info tab in Registration: Insurance as Auth Complete?, an alert will appear upon saving the charges warning users to review for a retro authorization prior to submitting a claim. No alert will be invoked, however, if the Auth Status is 1 - Auth not required.
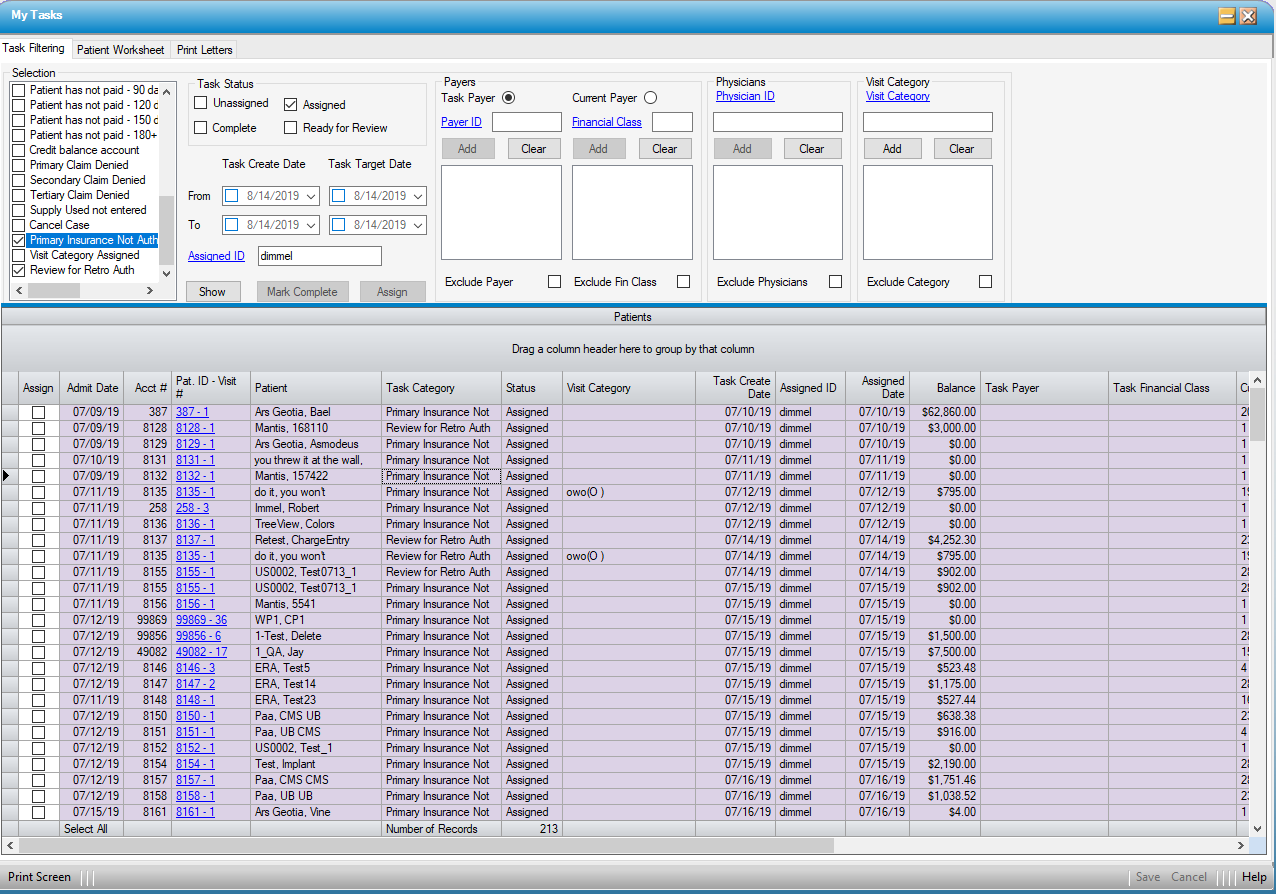
Workflow
If Primary Insurance Not Authorized and/or Review for Retro Auth have been selected in Workflow Configuration, then Workflow tasks will be created when the required conditions are not met.
Primary Insurance Not Authorized will create a Workflow task if the Auth Status is 0 - None or 3 - Auth Pending. The tasks will auto close if/when the Auth status is changed to indicate that authorization was completed, not required, or denied.
Review for Retro Auth will create a Workflow task if the Auth Status is not 1 - Auth not required and CPT codes billed were not entered in the Authorization Info tab of Registration: Insurance. The tasks will auto close if the CPT codes are updated in the Authorization Info tab after following up with the payer and obtaining retroactive authorization for the CPT codes billed.